Ulcus cruris venosum – Venous Leg Ulcers
Emergence and therapy
Venous leg ulcers, also known as ulcus cruris venosum (Latin: ulcus = ulcer, crus = lower leg, vena = blood vessel), refer to deep wounds that heal poorly and mainly occur in the ankle region and lower leg. The term “venosum” relates to the origin of the condition: an ulcus cruris venosum develops as a result of circulatory disorders that cause tissue damage in the skin and subcutaneous tissue. Thrombosis or chronic venous insufficiency (CVI) is often responsible for this condition. CVI refers to the cumulative clinical changes in the skin and subcutaneous tissue that occur within a chronic venous disease. An ulcus cruris represents the most severe form of this progression.
Symptoms
Visible symptoms and warning signs of CVI include increased pigmentation of the skin (brown patches) and vascular markings that extend in a spiderweb-like pattern over the inner edge of the foot and the inner ankle (corona phlebectatica). Persistent tissue damage caused by CVI can lead to ulcer-like and poorly healing wounds. In severe cases, such a venous leg ulcer can also result in necrosis of the skin tissue. This process can be accompanied by intense and painful discomfort.
Causes
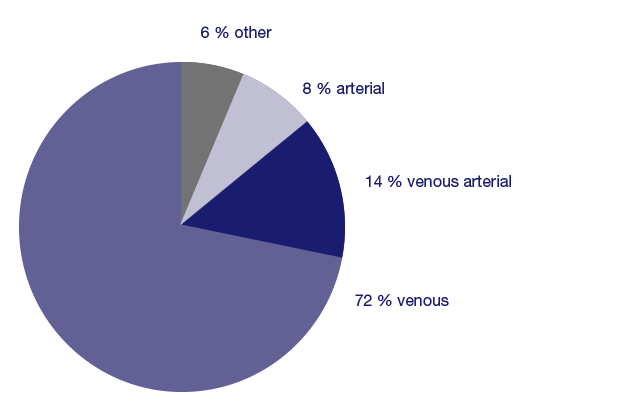
In 72% of cases, venous insufficiency (venous leg ulcer) is the main cause of a leg ulcer and an additional 14% of cases involve venous insufficiency (mixed leg ulcer). Other causes such as arterial circulatory disorders (peripheral arterial occlusive disease, PAD) and conditions like rheumatism, metabolic disorders (e.g., diabetes mellitus), and infections can also contribute to the development of leg ulcers.





